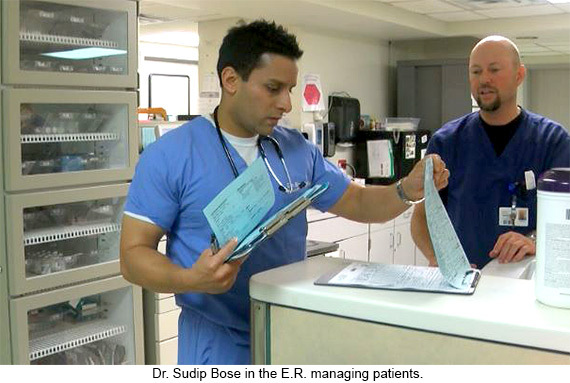
By Dr. Sudip Bose, MD, FACEP, FAAEM
There are many reasons why emergency rooms are dangerously overcrowded. With millions of Americans lacking adequate access to primary care providers, emergency rooms have become the primary health care system and safety net for the uninsured, underinsured and those without access to other medical care. Overcrowded and with overworked staffs, ERs are perilously close to collapse in many places. (See my other article on ERs here: Our Nation’s Emergency Rooms). In fact, many already have closed their doors. There is an increased demand for emergency department care, as hospital emergency rooms have experienced a 32 percent increase in patient volume over the past decade.
There are many reasons why we are seeing an influx in the volume of people seeking care in the ER. For starters, the fastest-growing age group in the United States is those over age 65, according to the 2010 US Census, and emergency room visits by the elderly are rising at an alarming rate. We also have a shortage of primary care physicians, and a growing percentage of health care practitioners that do not accept Medicare and Medicaid because of low reimbursement rates. Confounding those issues is the EMTALA (Emergency Medical Treatment and Active Labor Act) of 1986, which requires emergency rooms to treat all comers, regardless of urgency or income. Two-thirds of emergency visits occur after business hours, when doctors’ offices are closed. For people who find themselves in distress without access to care for these various reasons, the emergency room is often the only place to turn, and the double doors will always be open for them.