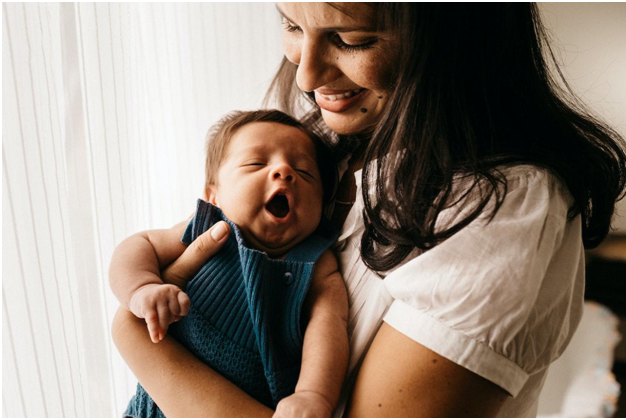
A woman’s pregnancy is divided into three trimesters. During each trimester, moms-to-be will encounter various changes in their bodies. However, most people don’t talk about the first few months after having a baby, which is commonly called the fourth trimester. While you won’t experience pregnancy symptoms anymore, there are still unique challenges you could encounter after the baby arrives. Dr. Bose explains five potential changes you may encounter once you bring your baby home.
1. Discomfort
Whether you give birth vaginally or via a C-section, you will experience some discomfort while you recover. Don’t be afraid to ask friends or family members to help you keep up with daily chores so you can focus on recovering. Get as much sleep as possible and focus on consuming a nutritious diet so that you can get back on your sleep feet quickly.
2. Larger Breasts
You gain weight during pregnancy, so it makes sense that your breasts become larger. If you are breastfeeding after the baby is born, your bust size may become even larger. Using a comfortable nursing bra is crucial for giving you the support you need and minimizing discomfort. If you already have a larger bust, you may worry that finding something for your pregnancy changes will be difficult. However, buying bras for large bust sizes is easy when you visit online shops that specialize in postpartum bras for larger busts. Rather than put yourself through the inconvenience of shopping in person, check out popular online retailers where you typically purchase diapers and wipes and add a few high-quality nursing bras to your shopping cart.
3. Hormones
It takes a while for your hormone levels to balance out after having a baby. You may find that you are more emotional than usual after your baby is born. This is normal. You can accommodate hormonal shifts by talking with your doctor and striving to practice self-care while adjusting to having a new baby in the house. What’s important to pay attention to is whether you begin to have symptoms of postpartum depression. If you start to notice extended bouts of sadness, lethargy, anxiety or appetite issues, it’s important to speak to your doctor right away.
4. Sleep Deprivation
According to one study, 11% of Americans experience chronic sleep deprivation. For new moms, this problem is much more prevalent because newborn babies wake several times each night to feed. Even if you try to sleep during the day while the baby naps, you will likely be exhausted during the first few months. You can minimize your fatigue by accepting help with other areas of your life and taking measures to improve the quality of your sleep.
5. Work/Life Balance
Your work/life balance will not be the same once your baby arrives. You will have several months off for maternity leave, but once you return to work, you must find a way to balance work responsibilities with raising your child. Communicating transparently with your clients and coworkers is a good way to establish your boundaries and let people know that you will not be quite as available as you once were. If you find that you need help managing administrative tasks, consider working with a virtual assistant.
Becoming a new mother is a wonderful experience, but the translation is not always simple. Even if you do not experience postpartum depression, there are still challenges you will face during the fourth trimester, especially if you plan to breastfeed and intend to start working soon after your baby arrives. Knowing what these difficulties are and how to combat them is important for living your best life for you and the baby.